Your chronic health issues like high blood pressure and fatigue are not isolated problems; they are being actively fueled by a silent, 24/7 infection in your mouth.
- Oral bacteria create a constant “inflammatory burden” that sabotages your body’s ability to regulate blood pressure and blood sugar.
- Treating gum disease is not just about saving your teeth; it’s a critical step to improving your overall health outcomes and making your other treatments more effective.
Recommendation: Stop viewing your oral health as separate. An immediate, comprehensive periodontal evaluation is the first step to breaking this cycle of systemic sabotage.
You’ve been diligent. You monitor your blood pressure, try to eat better, and follow your doctor’s advice. Yet, your numbers remain stubbornly high, and a persistent fatigue dogs your days. It feels like you’re fighting a battle on multiple fronts. We’re often told to look at diet, stress, or exercise as the primary culprits for these issues. We track our steps, count calories, and manage stress, all while ignoring a critical battlefield: our mouth.
The occasional bleeding when you brush? That faint redness in your gums? For many middle-aged adults, these are dismissed as minor annoyances. But what if they are not minor at all? What if they are signals of a low-grade, chronic war your body is waging 24/7? This isn’t just about dental hygiene anymore. This is about systemic health, and the evidence is becoming undeniable.
The true key to unlocking better health might not be another diet or a new exercise plan, but finally addressing the silent inflammation originating in your gums. This article will dismantle the artificial wall between oral and overall health. We will explore the shocking mechanisms through which your gum health is actively sabotaging your blood pressure, draining your energy, and impacting everything from your blood sugar to your cognitive function. It’s time to understand the source of the fight to finally win the war.
This guide breaks down the critical connections between your oral health and systemic well-being, providing a clear roadmap to understanding the risks and, more importantly, the solutions available right here in Montreal. Explore the sections below to uncover how this hidden battleground impacts your entire body.
Summary: Could Your Bleeding Gums Be the Reason for Your High Blood Pressure?
- How Treating Gum Disease Can Lower Your HbA1c Levels?
- Why Gingivitis Is a Risk Factor for Pre-Term Birth?
- The Bacteria in Your Gums Found in Alzheimer’s Brain Tissue?
- How Oral Bacteria Travel to Your Heart Valves?
- Is Your Body Tired from Fighting a Low-Grade Mouth Infection 24/7?
- Can You Reverse Periodontal Disease Once Bone Loss Has Started?
- Are Dental Implants a Safe Option for Seniors Over 70 in Montreal?
- How Treating Gum Disease Can Lower Your HbA1c Levels?
How Treating Gum Disease Can Lower Your HbA1c Levels?
The link between gum disease and diabetes is not a coincidence; it’s a destructive feedback loop. For anyone managing or at risk of Type 2 diabetes, controlling HbA1c levels—a key indicator of long-term blood sugar—is a constant focus. What is often overlooked is that a chronic infection in your gums can make this task significantly harder. The persistent inflammation from periodontitis increases the body’s systemic inflammatory burden, which in turn promotes insulin resistance. When your cells become resistant to insulin, your body has to work harder to manage blood sugar, causing your HbA1c levels to rise.
Treating gum disease, therefore, is not just a dental issue; it’s a diabetes management strategy. By eliminating the chronic infection in the mouth, you reduce the overall inflammation in your body. This allows your system to become more sensitive to insulin again, making your blood sugar easier to control. The impact is measurable and significant. Evidence shows that professional periodontal treatment can have a direct, positive effect on glycemic control.
In fact, the results can be comparable to adding a new medication to your diabetes regimen. A comprehensive Cochrane review of 30 studies shows a 0.43% reduction in HbA1c levels just 3-4 months after periodontal treatment. This demonstrates that addressing your oral health is a powerful, non-pharmacological way to support your diabetes care and lower your risk of complications.
Why Gingivitis Is a Risk Factor for Pre-Term Birth?
The systemic impact of gum disease extends to the most critical stages of life, including pregnancy. While hormonal changes during pregnancy can make gums more sensitive, persistent gingivitis or periodontitis is more than just a temporary discomfort. It represents a significant risk factor for adverse pregnancy outcomes, including pre-term delivery and low birth-weight babies. The same inflammatory mechanisms that affect blood pressure and blood sugar are at play here. The body’s inflammatory response to oral bacteria can trigger contractions and early labor.
For expectant mothers in Montreal, this information is vital. According to Health Canada, up to 50% of pregnant women experience gingivitis, making proactive oral care an essential part of prenatal health. The bacteria and the inflammatory mediators they produce can travel from the mouth, through the bloodstream, to the placenta, potentially impacting fetal development. It’s a stark reminder that a localized infection is rarely just local.

As Health Canada highlights, the precise pathway is still under intense study, but the association is clear. As they note in their guidance on oral health during pregnancy:
Periodontitis has also been associated with poor pregnancy outcomes such as having a pre-term delivery or a low birth-weight baby. However, how periodontitis may lead to these poor outcomes is not yet fully understood.
– Health Canada, Oral health and pregnancy – Canada.ca
This underscores the importance of integrating dental check-ups into routine prenatal care to mitigate risks and ensure the health of both mother and child.
The Bacteria in Your Gums Found in Alzheimer’s Brain Tissue?
Perhaps one of the most alarming connections being explored is the link between periodontal disease and neurodegenerative conditions like Alzheimer’s disease. This moves the conversation from cardiovascular and metabolic health to the very core of our identity: our cognitive function. The theory centers on a specific, highly destructive bacterium known as Porphyromonas gingivalis, a key pathogen in chronic periodontitis. This isn’t just any bacteria; it’s a particularly insidious actor capable of surviving and manipulating our immune system.
The hypothesis is that *P. gingivalis* can migrate from the mouth to the brain. This could happen through two primary routes: either by directly infecting cranial nerves, such as the trigeminal nerve, or by traveling through the bloodstream, eventually crossing the blood-brain barrier. Once in the brain, these bacteria and the toxic enzymes they release (called gingipains) can trigger neuroinflammation. This chronic inflammation is a hallmark of Alzheimer’s disease and is believed to contribute to the formation of amyloid-beta plaques, the protein clumps that disrupt brain function.
While research is ongoing and a direct causal link is not yet definitively proven, the evidence is mounting. Studies have found the DNA of *P. gingivalis* and its toxic gingipains in the brain tissue of deceased Alzheimer’s patients. This suggests that the oral microbiome is a far more influential factor in brain health than previously imagined. The idea that protecting your brain could start with protecting your gums is a paradigm shift, reframing dental care as a long-term strategy for cognitive preservation.
How Oral Bacteria Travel to Your Heart Valves?
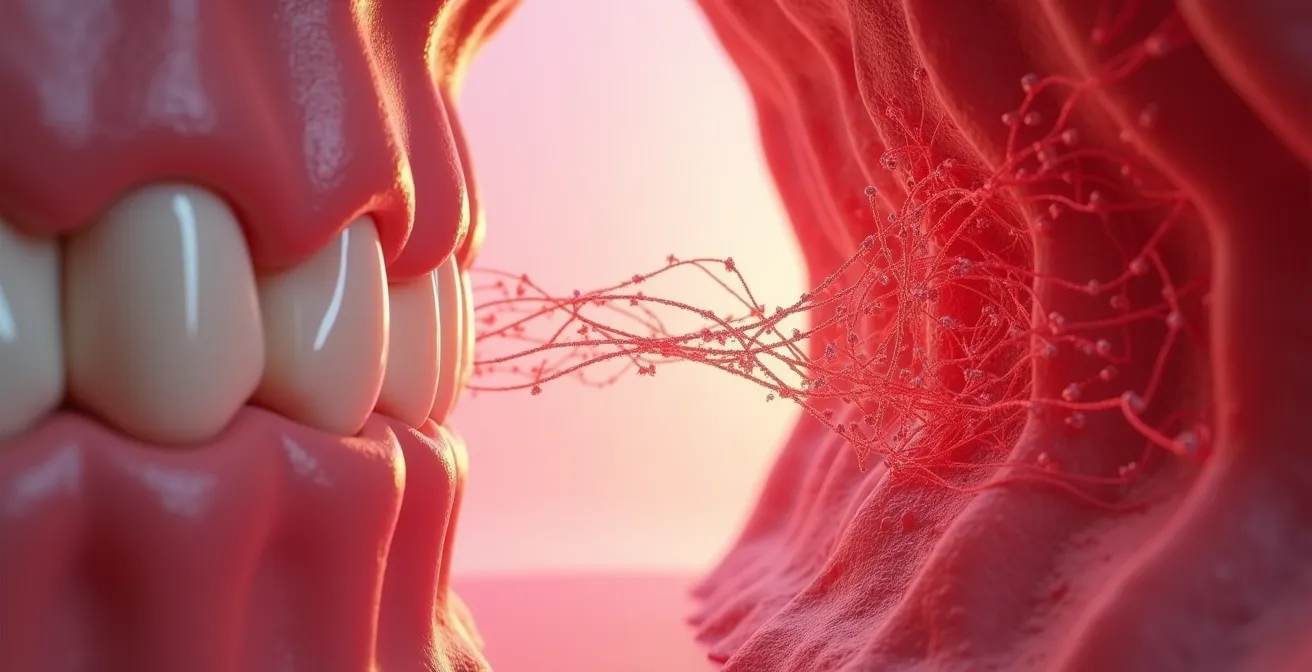
The link between your mouth and your heart is not metaphorical; it’s a physical pathway. Your circulatory system, a vast network of vessels, can become a highway for harmful bacteria if the barriers in your mouth are breached. When you have periodontitis, your gums are inflamed, ulcerated, and bleed easily. These tiny, chronic wounds create direct entry points for oral bacteria into your bloodstream. Every time you chew, brush, or even just have a routine dental cleaning, you can trigger a transient “bacteremia”—a brief shower of bacteria into your circulation.
This is where the direct sabotage of your cardiovascular health begins. These bacteria, particularly strains like *Porphyromonas gingivalis*, don’t just go for a joyride. They are active agents of inflammation. As they travel, they can attach to the walls of your blood vessels, including the coronary arteries, contributing to the formation and instability of atherosclerotic plaques. This is the underlying process of heart disease. Furthermore, they can directly reach the heart valves, leading to a dangerous condition called infective endocarditis, especially in individuals with pre-existing heart conditions.

The statistical evidence is stark. The inflammatory burden from gum disease puts a direct strain on your entire cardiovascular system, forcing it to work harder and making it more difficult to control hypertension. According to research highlighted by the American Heart Association, this isn’t a minor risk. As lead author Eva Muñoz Aguilera, D.D.S., M.Clin.Dent., explained:
Individuals with gum disease were twice as likely to have high systolic blood pressure values ≥140 mm Hg, compared to people with healthy gums (14% and 7%, respectively)
– Eva Muñoz Aguilera, D.D.S., M.Clin.Dent., American Heart Association Journal
This data confirms that people with periodontitis are twice as likely to have high blood pressure, making gum health a non-negotiable factor in cardiovascular care.
Is Your Body Tired from Fighting a Low-Grade Mouth Infection 24/7?
That persistent feeling of fatigue, the brain fog that lingers, the sense that you never fully recover—you might blame it on stress, age, or a long Montreal winter. But what if the source is a constant, low-grade battle your immune system is fighting every second of every day? Chronic periodontitis is exactly that: a 24/7 battle. Your body is perpetually trying to contain an infection that never goes away. This constant immune activation consumes a tremendous amount of energy and resources, leaving you feeling drained and exhausted.
This isn’t just a feeling; it’s a physiological reality. The chronic inflammation from your gums elevates systemic inflammatory markers throughout your body, like C-reactive protein (CRP). This state of constant inflammation puts a direct and measurable strain on your entire system, particularly your cardiovascular system. The effect on blood pressure is not hypothetical; it’s quantifiable. Groundbreaking research published in the Hypertension journal found a 5 mm Hg higher systolic blood pressure in patients with generalized bleeding gums compared to those with healthy gums. This is a significant increase that directly impacts your risk of heart attack and stroke.
Your body is tired because it’s diverting precious resources to fight a war in your mouth, a war that is simultaneously making your heart work harder. It’s the ultimate resource drain, sabotaging both your energy levels and your cardiovascular health. It’s time to connect the dots between how your mouth feels and how your body performs. The following checklist can help you self-assess if this silent battle might be affecting you.
Your Montreal Fatigue & Oral Health Self-Assessment
- Check for any sign of blood on your toothbrush or in the sink after your morning routine.
- Notice if that “morning brain fog” seems to persist longer than the typical Montreal winter fatigue you’re used to.
- Track your energy levels. Do you experience a significant slump in the afternoon that feels disproportionate to your day’s activities?
- Monitor for physical signs of tension. Do you notice an increase in jaw clenching or tightness, especially during stressful commutes on the Decarie?
- Assess your recovery. Does a relaxing weekend walk up Mont-Royal fail to restore your energy levels the way it used to?
Can You Reverse Periodontal Disease Once Bone Loss Has Started?
Hearing the term “bone loss” can be frightening. It sounds permanent and irreversible, leading many to feel that it’s too late to act. This is a critical point to clarify: while the bone that has already been lost due to periodontitis cannot be regrown naturally, the progression of the disease can absolutely be stopped. The goal of modern periodontal treatment is to halt the disease process, eliminate the infection, and create an oral environment that you can maintain to prevent any further damage. The idea that nothing can be done is a dangerous myth that leads to inaction and, ultimately, tooth loss.
The prevalence of advanced disease is alarming; for instance, a 2024 clinical study found that a staggering 82% of diabetic patients had Stage III or IV periodontitis, which involves significant bone loss. This underscores the urgency of intervention. Treatment for advanced periodontitis involves deep cleaning procedures (scaling and root planing) to remove the bacterial deposits below the gum line. In some cases, surgical procedures may be necessary to reduce the depth of periodontal pockets and facilitate effective cleaning. These interventions remove the source of the infection, which stops the inflammatory process that destroys the bone.
Failing to address this is not a passive choice. It has active, negative consequences for your overall health. The systemic inflammation continues unabated, undermining other medical treatments. For example, a major retrospective study showed periodontitis was associated with a 20% higher risk of unsuccessful antihypertensive treatment. In other words, your untreated gum disease is actively working against your blood pressure medication. Reversing the *disease process* is not just possible; it is essential to allow your body—and your medications—to work effectively.
Are Dental Implants a Safe Option for Seniors Over 70 in Montreal?
After successfully halting periodontal disease, many seniors in Montreal face the challenge of replacing lost teeth. Dental implants have become the gold standard for tooth replacement, offering unparalleled stability and function. However, patients over 70 often wonder if implants are a safe and viable option for them, especially if they are managing other health conditions like hypertension. The answer is overwhelmingly yes, provided there is careful planning and collaboration between your dentist, your periodontist, and your general practitioner.
The primary consideration for implant success is not age, but overall health and the quality of the jawbone. While healing may take slightly longer in older adults, success rates remain very high, typically between 90-95%. The key is ensuring that any systemic conditions, especially hypertension, are well-managed. This is a critical point, as CardioSmart, the American College of Cardiology’s patient platform, reports that less than 50% of hypertensive patients have their condition under control. Proceeding with surgery without controlled blood pressure is a risk. Therefore, a pre-surgical consultation with your GP is essential to ensure your health is stable.
For Montreal seniors, there are also practical considerations, including healing times and RAMQ coverage. The table below outlines key differences between a standard adult case and a senior over 70 in Montreal.
| Factor | Standard Adult | Seniors 70+ Montreal |
|---|---|---|
| Healing Time | 3-6 months | 4-8 months |
| Medication Interactions | Minimal | Requires GP coordination |
| RAMQ Coverage | Not covered | Partial dentures covered |
| Success Rate | 95-98% | 90-95% with proper care |
This table highlights that while some aspects require more careful management, dental implants are a predictable and highly successful solution for restoring function and quality of life for seniors, as long as a comprehensive, team-based approach is taken to manage both oral and systemic health.
Key Takeaways
- Chronic gum inflammation is a major contributor to systemic health issues, including high blood pressure and insulin resistance.
- Treating periodontitis is not just a dental concern; it’s a direct intervention to improve your cardiovascular and metabolic health.
- The link is physical: oral bacteria enter the bloodstream and travel throughout the body, causing a constant, resource-draining inflammatory response.
How Treating Gum Disease Can Lower Your HbA1c Levels?
We’ve established the mechanism: treating gum disease reduces systemic inflammation, which improves insulin sensitivity. But what does this look like in the real world? The results can be life-changing. It’s about moving from theory to tangible health improvements. The fight against high HbA1c levels is often a frustrating journey of incremental changes, but addressing oral health can provide a significant breakthrough. It is one of the few interventions that can simultaneously improve multiple health markers at once.
Consider the powerful findings from a recent study. A 2024 study from Tokyo Medical University tracked diabetic patients with severe periodontitis. At the beginning of the study, their average HbA1c was a dangerously high 9.6%. After six months of intensive diabetes care combined with simple professional dental cleanings (prophylaxis), their average HbA1c dropped to 7.4%. This dramatic improvement was directly correlated with the improvement in their gum health. It wasn’t just about the diabetes treatment; it was the combined-arms assault on both the metabolic and the inflammatory fronts that made the difference.
This provides a clear and hopeful path forward. Your efforts to control your blood sugar are not in vain, but they may be hampered by a hidden enemy. By eliminating the chronic inflammatory burden from your mouth, you are not just saving your teeth—you are unlocking the full potential of your other health strategies. You are removing the saboteur from within your own system, allowing your body to finally heal and regulate itself more effectively. This is the essence of integrative health: understanding that no part of the body works in isolation.
The evidence is clear: the health of your mouth is inextricably linked to the health of your body. To stop the systemic sabotage, the first step is a comprehensive periodontal evaluation to understand your specific level of inflammatory burden. Schedule a consultation today to take control and put an end to this silent, 24/7 battle.