General Dental Care
Your mouth is far more than a gateway for food and conversation—it’s a complex ecosystem that directly influences your cardiovascular health, immune function, and even cognitive longevity. Yet despite brushing twice daily, many Montrealers unknowingly harbor silent periodontal inflammation or miss critical signs of decay between dental visits. General dental care encompasses not just the two minutes you spend with a toothbrush, but a comprehensive understanding of prevention strategies, professional interventions, and the biological mechanisms that determine whether your teeth last a lifetime or require costly restoration.
This resource connects the essential pillars of oral health into a coherent framework. From optimizing your morning routine and understanding what truly happens during a scaling appointment, to recognizing when jaw pain constitutes a true emergency versus a wait-able issue, you’ll gain practical insights grounded in clinical protocols used across Montreal dental practices. Whether you’re troubleshooting persistent bleeding gums, evaluating therapeutic rinse options, or simply questioning if your current routine delivers actual protection, the following sections provide the evidence-based foundation you need.
Why Daily Oral Care Forms Your Long-Term Health Foundation
The average person spends roughly 38 days brushing their teeth over a lifetime, yet many never learn the physiological rationale behind the ritual. Daily oral hygiene isn’t about aesthetics or fresh breath—it’s a biological intervention against bacterial colonization. When you skip even one evening session, plaque biofilm matures from soft, brushable deposits into organized communities that secrete acids and inflammatory toxins.
A cost-effective long-term routine requires three non-negotiable components: mechanical disruption of plaque, chemical reinforcement of enamel, and interdental cleaning. The sequence matters more than most realize. Brushing immediately after acidic foods (citrus, coffee) can actually abrade softened enamel—waiting 30 minutes allows saliva’s natural buffering to restore your mouth’s pH balance first. Similarly, the debate over whether to rinse after brushing hinges on fluoride contact time: rinsing immediately washes away the protective mineral coating before it can integrate into enamel.
For Montreal residents managing hard municipal water, mineral buildup on toothbrush bristles can reduce cleaning efficiency. Replacing your brush every 10-12 weeks—not when bristles splay, but based on bacterial accumulation invisible to the naked eye—prevents reintroducing yesterday’s pathogens. Travel maintenance poses another challenge: portable UV sanitizers popular in Canadian outdoor stores offer minimal benefit compared to simply air-drying bristles between uses, as moisture breeds bacteria far more than brief environmental exposure.
What Actually Happens During Professional Dental Cleanings
Professional prophylaxis addresses the fundamental limitation of home care: calculus adhesion physics. Once plaque mineralizes into tartar through salivary calcium incorporation, its crystalline structure bonds to enamel with a tenacity that manual brushing cannot overcome. The calcified matrix acts like barnacles on a ship hull, providing protected real estate for anaerobic bacteria to colonize below the gumline where oxygen-rich saliva can’t reach.
Dental hygienists in Quebec use two primary scaling approaches:
- Manual curettes: Angled metal instruments that require tactile precision to navigate root contours, ideal for isolated deposits and patients with sensitivity to vibration
- Ultrasonic scalers: Devices generating 25,000-50,000 vibrations per second through a water-cooled tip, fragmenting calculus through cavitation bubbles while simultaneously flushing debris
- Combination protocols: Starting with ultrasonic for bulk removal, then hand-finishing subgingival areas for smooth root surfaces that resist future bacterial adhesion
The appearance of blood during scaling doesn’t indicate tissue damage—it reveals existing inflammation. Healthy gingival tissue doesn’t bleed under professional instrumentation. When hygienists encounter bleeding, they’re essentially diagnosing periodontal infection hiding beneath seemingly normal pink tissue. This is why cleaning frequency should follow individual risk profiles rather than arbitrary six-month intervals. Patients with diabetes, immunosuppression, or genetic predisposition to aggressive periodontitis may require quarterly maintenance, while those with excellent home care and stable biometrics might extend to eight or nine months safely.
The Hidden Connection Between Gums and Overall Health
Recent research from McGill University’s Faculty of Dentistry has reinforced what clinicians have observed for decades: periodontal inflammation functions as a chronic systemic stressor. The same bacterial endotoxins that destroy jaw bone enter the bloodstream through ulcerated gum pockets, triggering immune responses far from the mouth.
The diabetes-periodontitis relationship operates as a vicious cycle. Elevated blood glucose creates a sugar-rich environment in gingival fluid, feeding pathogenic bacteria. Simultaneously, inflammatory cytokines from infected gums promote insulin resistance, making glucose control harder. Quebec endocrinologists now routinely recommend dental evaluations for patients struggling with A1C management, recognizing that treating gum disease can improve metabolic markers as significantly as medication adjustments.
Pregnancy outcomes represent another critical connection. Pregnant individuals with untreated periodontal disease face elevated risk of preterm birth and low birth weight—complications that strain neonatal resources across Montreal’s hospital network. The mechanism involves inflammatory prostaglandins that can trigger early labor. Obstetric guidelines from the Society of Obstetricians and Gynaecologists of Canada now include second-trimester dental screening as a standard prenatal care recommendation.
Emerging Alzheimer’s research has identified Porphyromonas gingivalis—a keystone periodontal pathogen—in brain tissue of dementia patients. While causation remains unproven, the correlation suggests that decades of low-grade oral infection may contribute to neuroinflammation and cognitive decline. Cardiovascular strain follows similar pathways: bacterial DNA from oral pathogens has been recovered from atherosclerotic plaques, suggesting that daily gingival bleeding may seed arterial inflammation over years.
Understanding Tooth Decay Beyond the Sugar Myth
While candy consumption correlates with cavities, the true driver of carious lesions is pH balance, not sugar itself. Oral bacteria metabolize fermentable carbohydrates (including crackers, bread, and dried fruit) into lactic acid. When this acid drops your mouth’s pH below 5.5, enamel’s hydroxyapatite crystals begin dissolving—a process called demineralization.
Hidden interproximal decay—cavities forming between teeth—escapes visual detection until they’re advanced. The contact points where molars touch create oxygen-poor zones where acidogenic bacteria thrive undisturbed. Even diligent brushers who skip flossing develop these “stealth cavities” that only reveal themselves through bitewing radiographs during checkups. By the time you feel sensitivity or see a visible hole, decay has often penetrated through enamel into the softer dentin layer.
Your mouth possesses a natural repair mechanism: remineralization. Saliva contains calcium and phosphate ions that can rebuild early enamel damage, provided the pH returns to neutral quickly enough. This explains why sipping acidic beverages over hours causes more harm than drinking the same volume in 10 minutes—prolonged acid exposure prevents remineralization windows. Dry mouth conditions (xerostomia) sabotage this protective cycle, which is why medications with anticholinergic side effects—common antidepressants, antihistamines, and blood pressure drugs—dramatically increase cavity risk regardless of hygiene habits.
The genetics versus environment debate has nuanced answers. Some individuals inherit thinner enamel, deeper molar fissures, or altered saliva composition that affects buffering capacity. However, even genetic predisposition requires environmental triggers. Montreal’s fluoridated water supply (0.7 ppm) provides passive protection, but residents relying on well water or reverse osmosis filtration miss this community-wide safeguard and should discuss supplemental fluoride protocols with their dentist.
When Dental Situations Become True Emergencies
Montreal’s healthcare system creates unique challenges for dental crises. Unlike medical emergencies with 24/7 hospital ER access, dental urgent care follows fragmented after-hours protocols that many residents only discover mid-crisis. Understanding the distinction between true emergencies and wait-able issues prevents both unnecessary ER visits and dangerous treatment delays.
Genuine dental emergencies requiring immediate intervention include:
- Uncontrolled bleeding lasting beyond 20 minutes despite pressure application
- Facial swelling that impairs breathing, swallowing, or closes the eye—potential signs of spreading infection
- Trauma with tooth displacement where the tooth has been knocked completely out or pushed into the jaw
- Suspected jaw fracture following impact, indicated by malocclusion or inability to open/close the mouth
Conversely, conditions that feel urgent but can safely wait for next-business-day care include isolated toothaches without swelling, small chips without pulp exposure, or lost fillings that aren’t causing sharp pain. The financial pitfalls of mismanaged emergency care can be severe: a hospital ER visit in Quebec may cost $500-800 out-of-pocket for uninsured services, yet ER physicians typically only prescribe antibiotics and analgesics without definitive treatment, necessitating a follow-up dental appointment anyway.
Emergency dental clinics operating in Montreal neighborhoods like Plateau-Mont-Royal and Ville-Marie offer middle-ground options, providing same-day appointments for urgent issues at lower cost than hospital emergency departments. Before crisis strikes, identify which practices near your home or workplace offer emergency slots and verify their after-hours contact protocols.
A home emergency dental kit should contain sterile gauze, a small container with lid (for transporting an avulsed tooth in milk or saliva), over-the-counter pain relievers, ice packs, and temporary filling material available at pharmacies. For knocked-out permanent teeth, time dictates success: reimplantation within 30 minutes offers the highest survival rates. Rinse the tooth gently without scrubbing the root, attempt to reposition it in the socket if possible, and seek immediate care while keeping it moist.
How Clinical Sterilization Protocols Protect You
The instruments entering your mouth undergo a rigorous decontamination sequence that most patients never see but should deeply appreciate. Quebec’s regulatory framework, enforced by the Ordre des dentistes du Québec, mandates specific sterilization validations that exceed general medical device standards due to the blood-rich environment of oral procedures.
After each patient, reusable instruments travel through a defined pathway: initial pre-cleaning to remove gross debris, ultrasonic bath agitation to dislodge bioburden from crevices, inspection for residual contamination, packaging in heat-sealed pouches with chemical indicators, and finally autoclave sterilization using steam at 121°C for 30 minutes or 134°C for shorter cycles under pressure.
The autoclave validation process combines three monitoring levels: mechanical gauges confirming temperature and pressure parameters, chemical indicators that change color only when sterilization conditions are met, and weekly biological tests using heat-resistant spore strips cultured in a lab to verify actual microbial kill. Any failed biological test triggers a recall protocol requiring re-sterilization of all instrument loads processed since the last successful test—a costly but essential patient protection measure.
Water line safety represents a less visible concern. Dental unit waterlines, which supply the handpiece coolant and rinse water, can harbor biofilm if not properly maintained. Progressive Montreal practices have implemented daily flushing protocols and continuous low-level disinfectant systems to ensure water quality meets safe drinking standards, eliminating the risk of immunocompromised patients encountering opportunistic pathogens like Legionella or Pseudomonas.
The “open the bag” rule provides patient-facing verification: sterile instrument pouches should only be opened in your direct view immediately before use. If you observe pre-opened instruments on a tray or pouches that are torn, damp, or lack intact chemical indicators, you have every right to request confirmation of their sterility status before treatment proceeds.
Surface disinfection follows specific contact time requirements. The blue or pink solutions used to wipe dental chairs aren’t instantly effective—Health Canada-approved hospital-grade disinfectants require 2-10 minutes of wet contact depending on the product to achieve pathogen elimination. Reputable practices allow sufficient turnover time between patients for both surface disinfection and proper instrument reprocessing rather than rushing appointments.
Your oral health outcome depends on decisions made daily at home and periodically in the dental chair. By understanding the biological rationale behind prevention recommendations, recognizing the systemic implications of gum disease, and appreciating the safety infrastructure protecting you during professional care, you transform routine dental maintenance from a dreaded obligation into an informed health investment. Each topic introduced here—from interdental cleaning techniques and therapeutic rinse selection to root canal necessity and recession prevention—deserves deeper exploration based on your specific risk profile and concerns.

Why Is Prescription Mouthwash Limited to Two Weeks? A Patient’s Guide
If your dentist prescribed a chlorhexidine rinse like Peridex and stressed a two-week limit, there’s a critical medical reason. This time limit establishes a precise therapeutic window, allowing the rinse’s potent antimicrobial action to treat an acute issue like gingivitis…
Read more
Mouthwash for Bad Breath vs. Gingivitis: Are You Using the Wrong One?
In summary: Stop choosing mouthwash based on the problem on the label; select it based on the active ingredient’s mechanism. Alcohol-based rinses can worsen bad breath by drying your mouth and disrupting your oral microbiome. For gum health (gingivitis), look…
Read more
Why Do 90% of Adult Cavities Start Between the Teeth?
Contrary to popular belief, persistent cavities between your teeth are not a sign of poor hygiene, but a spatial mapping failure. Standard brushing and simple flossing are ineffective against the unique ‘oral topography’ of gaps and contours where destructive plaque…
Read more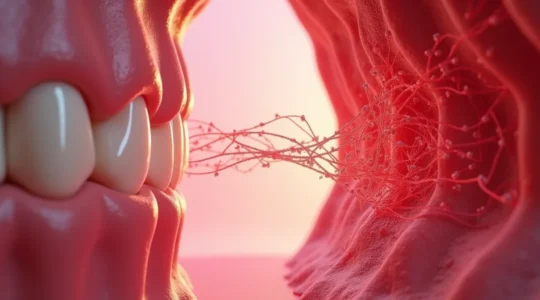
Could Your Bleeding Gums Be the Reason for Your High Blood Pressure?
Your chronic health issues like high blood pressure and fatigue are not isolated problems; they are being actively fueled by a silent, 24/7 infection in your mouth. Oral bacteria create a constant “inflammatory burden” that sabotages your body’s ability to…
Read more
Why Can’t You Remove Tartar at Home with a Pick from Amazon?
Attempting to remove tartar at home with a metal tool is not a risk; it is a guarantee of permanent damage to your teeth. Dental tartar has a mineral composition similar to concrete and forms a chemical bond with your…
Read more
Why Is Your Breath Bad Even Though You Brush Twice a Day?
Brushing twice a day isn’t a guarantee against bad breath; the real culprits are often the subtle, overlooked errors in your technique and timing. The tongue is a primary source of odor-causing bacteria that a toothbrush can’t effectively remove. The…
Read more
How Do You Know If Your Dentist’s Tools Are Truly Sterile?
True dental safety is not a feeling; it is a series of verifiable processes that you, the patient, can observe and question. Sterilization is only confirmed by biological spore tests, not just by the look of an instrument or a…
Read more
Why Do You Keep Getting Cavities Despite Brushing and Flossing?
If you’re meticulously brushing and flossing but still leaving dental check-ups with bad news, the problem isn’t your discipline—it’s your oral environment. The real culprits are often hidden factors like the frequency of your snacking, medication side effects creating dry…
Read more
Why Are Your Gums Receding Even Though You Brush Twice a Day?
Your gum recession isn’t a failure of diligence; it’s the result of hidden mechanical saboteurs that even the best brushing can’t fix alone. Aggressive brushing techniques and hard bristles cause direct physical trauma to your gum tissue. Underlying factors like…
Read more
How to Recover From a Root Canal in 24 Hours Without Complications?
In summary: A root canal is a mechanical cleaning; antibiotics only manage pre-op swelling and cannot cure the infection alone. Your first 24 hours are critical. Proactively manage inflammation with ice packs and stick to a soft-food diet to prevent…
Read more